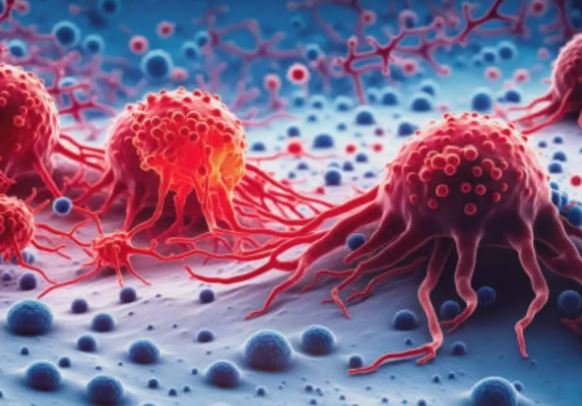
Stem cell therapy, particularly hematopoietic stem cell transplantation (HSCT), has significantly advanced the treatment landscape for various types of blood cancers. Here’s an overview of these advances and their impact:
Types of Stem Cell Therapy
- Autologous Stem Cell Transplantation (ASCT):
- Source: Uses the patient’s own stem cells collected from bone marrow or peripheral blood.
- Indication: Often used in lymphomas, multiple myeloma, and certain leukemias to allow high-dose chemotherapy or radiation therapy, followed by reinfusion of the patient’s own stem cells to restore blood cell production.
- Allogeneic Stem Cell Transplantation (allo-HSCT):
- Source: Involves stem cells from a compatible donor, typically a sibling or unrelated donor.
- Indication: Used when intensive chemotherapy or radiation is insufficient, or when the immune system needs replacement (e.g., acute leukemias, myelodysplastic syndromes).
Advances in Stem Cell Therapy
- Improved Donor Matching:
- HLA Typing: Advancements in human leukocyte antigen (HLA) typing and donor selection have improved compatibility and reduced the risk of graft-versus-host disease (GVHD).
- Reduced Intensity Conditioning (RIC):
- Less Toxic Preparative Regimens: RIC protocols allow older patients or those with comorbidities to undergo allo-HSCT by using lower doses of chemotherapy or radiation, reducing treatment-related toxicity.
- Targeted Conditioning Regimens:
- Specificity: Development of targeted conditioning regimens that selectively deplete malignant cells while preserving normal stem cells has improved outcomes and reduced complications.
- Graft Engineering:
- T-Cell Depletion: Techniques to selectively remove T-cells from the donor graft can mitigate the risk of GVHD.
- Manipulation: Genetic engineering or manipulation of donor stem cells to enhance graft-versus-leukemia (GVL) effects while minimizing GVHD is an area of active research.
- Cord Blood Transplantation:
- Expanded Use: Advances in cord blood banking and transplantation techniques have expanded the availability of this stem cell source, particularly for patients lacking matched related or unrelated donors.
- Post-Transplant Care and Supportive Therapies:
- Infection Management: Improved strategies for infection prevention and treatment post-transplant have reduced complications.
- Supportive Care: Enhanced supportive care measures, including nutrition management, pain control, and psychosocial support, contribute to better patient outcomes and quality of life.
Challenges and Future Directions
- GVHD and Immune Reconstitution: Despite advancements, GVHD remains a significant complication. Research continues into novel immunosuppressive agents and strategies to promote immune tolerance and reconstitution post-transplant.
- Relapse Prevention: Strategies to prevent disease relapse after HSCT, such as maintenance therapy, targeted therapies, and immunotherapies, are actively investigated.
- Personalized Medicine Approaches: Tailoring treatment based on genetic profiling of both the patient and the donor may optimize transplant outcomes and reduce complications.
Conclusion
Stem cell therapy, particularly HSCT, has revolutionized the treatment of blood cancers, offering curative potential for many patients who previously had limited treatment options. Ongoing research and clinical trials are focused on refining transplant techniques, improving outcomes, and expanding eligibility criteria to benefit more patients. As advancements in stem cell biology, immunology, and supportive care continue, the future holds promise for further enhancing the efficacy and safety of stem cell therapy in the treatment of blood cancers.

Here, you can discover a wide selection of slot machines from top providers.
Visitors can enjoy classic slots as well as modern video slots with stunning graphics and interactive gameplay.
If you’re just starting out or a seasoned gamer, there’s always a slot to match your mood.
no depisit bonus
All slot machines are instantly accessible 24/7 and designed for laptops and mobile devices alike.
You don’t need to install anything, so you can jump into the action right away.
Platform layout is intuitive, making it convenient to find your favorite slot.
Register now, and enjoy the world of online slots!